Bright Futures
Articles and Updates from Phoenix Children's
Samantha Arko wears her color-coded hospital ID wristbands long after leaving the hospital. They serve as a fashion statement, a badge of honor and a conversation starter to raise awareness about ulcerative colitis.
“I have a lot of them,” said Samantha.
“She doesn’t like to cut them off after she leaves the hospital,” added her mother, Nichole Arko.
Color-coded wristbands notify hospital care providers of important patient details. Some are red allergy alerts (Samantha is allergic to cashews and hazelnuts). The white bands have scannable codes that access medical records and patient details. Still others may be green, blue or other colors standardized by hospitals for medical conditions.
They remind 10-year-old Samantha of successfully navigated checkpoints along her unexpected “frequent flyer” journey at Phoenix Children’s. That journey has earned her national attention for helping other kids with her disease.
“I really know my way around the hospital,” said Samantha, “from doctors’ offices and clinics to surgery and infusion centers.”
Her journey began when Samantha was 8 years old. In August of 2021 she got a crash course in the ABCs of IBD – inflammatory bowel disease. The immune-system disease triggers chronic inflammation (redness and swelling), causing gastrointestinal (GI) tract damage. Sometimes inherited, its exact cause is unknown. Although not curable, treatment helps manage symptoms.
Crohn’s disease and ulcerative colitis are the main types of IBD. Samantha has ulcerative colitis. It causes colorectal (colon and rectal) lower intestinal inflammation, while Crohn’s can affect any part of the GI tract. IBD symptoms can include belly pain, rectal bleeding and bowel incontinence, an urgent need to have a bowel movement.
A third grader’s school year gets off to a bad start
One of Samantha’s more embarrassing experiences happened on her first day back to school, before her IBD diagnosis. Classroom activities were interrupted by her mad dash for the bathroom.
Earlier that month, Samantha had dismissed random symptoms at home. They included light blood or mucous in the stool, feeling “gassy” and sudden urges to need the bathroom. But symptoms were mild and occasional, so she didn’t worry. After her unpleasant school-day experience, Samantha’s symptoms quickly escalated to more obvious rectal bleeding and GI discomfort.
Looking for answers
Samantha’s pediatrician suspected ulcerative colitis.
“That was the first time I’d heard of it,” said Nichole. They were referred to a gastroenterologist (GI specialist). Brad Pasternak, MD, scheduled a magnetic resonance enterography (MRE), which provides detailed intestinal pictures. Samantha also had a diagnostic colonoscopy. Doctors examine the colon using a long, flexible tube and tiny, lighted camera.
Samantha said she had “a bunch” of tests including blood draws, stool samples, imaging tests and lab work. The day before the colonoscopy, she fasted from solid food and took colon-clearing laxatives. The 30-minute, same-day procedure required general anesthesia.
“I stayed calm because it’s not going to help if you’re crying,” recalled Samantha. “It was hard, but I tried to think of good things like knowing this will lead to answers.”
Dr. Pasternak confirmed an ulcerative colitis diagnosis. It would change life for their busy Phoenix-based family. Nichole and her husband, Mike, are proud parents of two daughters and fans of Scruffy, the family’s dog.
Natalie — her sister one year older than Samantha — loves school and theater. Her credits include playing Ariel in The Little Mermaid and Olaf in Frozen. A student council member, Samantha loves math, reading and science. She’s a club soccer player and Girl Scout. Their full schedules soon became even busier.
A family’s detour into uncharted territory
After her diagnosis, symptom flare-ups and medical appointments interrupted daily activities.
“It was overwhelming,” said Nichole. “You’re trying to understand this condition and how to help your child. The first year was really challenging, trying to find the right medication.”
Samantha took oral steroids at first to ease inflammation. It made her cheeks puffy and required a Dexa scan to rule out bone complications. She later started oral medication, which failed after six weeks. Injectable medicine helped manage symptoms for a year before failing.
“Every four to six months, we had to increase the dose or try a different medication,” said Nichole.
Samantha visits Phoenix Children’s infusion center every six weeks for IV therapy. It’s working, but Samantha worries about a relapse.
New things to learn and new friends to lead the way
Samantha felt scared at first, yet lucky to have support.
“Everyone’s been great,” said Samantha. “We take things one day at a time.”
She appreciates Dr. Pasternak and others at Phoenix Children’s who make their lives a little easier.
“At first, I’m wary about new doctors,” said Samantha. “Will they be friendly, harsh or not like to talk? I got to know Dr. Pasternak very well, very quickly. He’s always part of things. It’s nice to see him at activities and events – not just in his hospital scrubs and mask.”
“Dr. Pasternak responds to our questions or concerns,” added Nichole. “He’s helped educate Mike and me, and he’s always supportive. We’re lucky to have a world-class hospital in our backyard.”
A painful new puzzle to solve
In late 2023, Samantha began having sharp pain on one side or in the middle of her stomach. She’d feel sudden stabs of pain while reading a book, watching TV or going for a walk.
“Sometimes, the pain wakes me up early in the morning,” said Samantha.
“Her dad and I traded shifts staying with Samantha at night,” added Nichole, “so one of us could get a good night’s sleep.”
Diagnosing new symptoms required another colonoscopy – her fourth to date – and a CT scan. Samantha was once again waiting for answers.
“There are a lot of maybes, but you have to stay strong,” said Samantha.
A purple star continues to rise, lighting the way for others
After her diagnosis, Samantha thought of other kids who may feel lonely, scared or embarrassed about IBD.
“I wanted to help others,” said Samantha. “Dad is on a lot of boards, and I thought, ‘I could do that.’”
In 2022, Samantha founded the IBD Junior Board at Phoenix Children’s to raise awareness, support IBD kids and fund research for a cure.
“I wanted it to be run by kids,” Samantha said.
With just eight kids, they raised over $7,000 the first year. Their membership and successes keep growing. They create logos and T-shirt designs for fundraising and awareness hikes. They arrange video tournaments and plan toy drives for IBD-hospitalized kids. Samantha encourages “welcome distractions” like soft, huggable Squishmallows® or activity books.
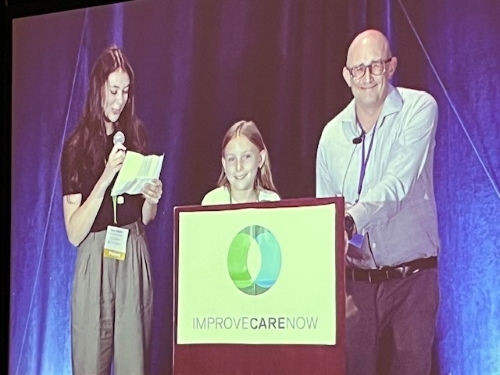
Samantha is a star among family, friends and IBD Junior Board supporters, but she’s always a team player. At the age of 10, Samantha joined Dr. Pasternak on a Louisville hotel ballroom stage to address a national pediatric gastroenterology conference.
Video of Samantha's speech with Dr. Pasternak at the Improve Care Now conference in Louisville KY, October 2023: Creation and Benefit of a Patient-Led IBD Junior Board.
“It was a proud moment,” said Nichole.
Samantha shared stories and talked about creating the board. They encouraged other children’s hospitals to start their own boards.
Samantha’s group wants local mayors to light up their communities in purple for IBD Awareness Day in May. They have big plans, and Samantha remains optimistic. She reminds others that every effort matters.
“If you want to make a difference,” Samantha said, “whatever you do, it counts.”